For the last three decades, kidney transplantation has been the preferred approach to renal replacement therapy for the vast majority of patients. The virtue of transplantation lies in the expected conferral of a longer quantity and a better quality of life to recipients than they would have from chronic dialysis.
Advances in the management of hypertension, diabetes, and other contributors to the burdens of cardiovascular morbidity have permitted more of our fellow citizens to live longer, surviving (or even avoiding) what would previously have been a fatal myocardial infarction or cerebrovascular accident, and thus surviving long enough to live with kidney failure. Demand for a transplantable kidney has tracked growth in the number of new patients with kidney failure, and pharmacologic advances have substantially attenuated what were once severe iatrogenic complications of systemic immunosuppression, making transplantation a plausible therapeutic possibility for more patients. But the supply of transplantable kidneys has not kept pace.
Extant Policy Approaches
There have been three non-mutually exclusive policy approaches to addressing the supply-demand problem: (1) increasing supply, (2) reducing demand, and (3) revising the allocation system. Despite aggressive, federally sponsored efforts to increase the supply of organs from deceased donors, growth in supply has come primarily from using more organs from so-called “expanded-criteria” donors (ECD) and donors after circulatory death (DCD). The total number of kidneys procured from standard-criteria (SCD) donors (read: young, healthy donors without comorbidities) has remained flat to falling over the last 5 years [1]. As a result, the total number of kidneys from all deceased donors transplanted in 2009 (7,248) is not substantially higher than in 2006 (7,178) [1]. Over the same interval, the total number of kidneys from living donors has remained stable at between 6,000 and 6,500 kidneys per year [2].
Paired kidney donation and donor “chains” initiated by a volunteer for nondirected living donation are recent, exciting innovations [3], but the total number of organs transplanted from these arrangements each year remains small [4]. Efforts to repeal existing legislation that prohibits policy experiments in remunerating prospective living donors have so far been unsuccessful [5] and are, at any rate, highly controversial.
While reducing demand for kidney transplants has not been thus far successful (prevalence rates of end-stage renal disease—ESRD—continue to rise [6]), some have argued that the total number of candidates on the waiting list substantially overstates the true demand [7-9]. Critics have pointed to the fact that a large fraction of patients on the waiting list are classified as “inactive,” or “status 7” in the parlance of United Network for Organ Sharing (UNOS) and the Organ Procurement and Transplantation Network (OPTN). Candidates listed as status 7 are not able to receive an organ offer but are able to accrue waiting time on the list so that, once “activated,” they can receive organ offers based on time accrued while they were inactive. Some patients listed as status 7 never become active and are ultimately removed from the waiting list. Therefore, status 7 patients represent a “shadow” demand, which tends to inflate (and overdramatize) the true demand for organs.
A candidate may be designated as status 7 for many reasons, candidates may switch back and forth between status 7 and active status with unknown frequency, and different transplant centers have substantially different policies regarding use of the status 7 designation. Patients may be designated as status 7 because of insurance ineligibility, a recent (reversible) illness, or because their renal function remains too good to benefit from transplant but sufficiently low to accrue waiting time. Some centers with large waiting lists and long median waiting times routinely list patients as status 7 after referral and then begin the evaluation process once the candidate has accrued sufficient waiting time to rise close to the top of the center’s list, thus reducing the need for and expense of repeated screening tests over a period of years.
To be sure, some fraction of these patients will never become active candidates and will be removed from the list due to physiologic deterioration or death. But a patient listed as status 7 at a center with a median waiting time that exceeds 5 years may well be a medically viable transplant candidate in the first or the fourth year of status 7 listing, and deteriorate and be removed after 5 years on the list. Far from being an instance of “shadow” demand, attrition of patients listed as status 7 is more plausibly understood as a feature of longer median waiting times to transplantation.
Finally, even if every patient listed as status 7 is not and never was a medically suitable candidate for transplantation, other research has shown that there are an additional 80,000-130,000 patients with ESRD who could theoretically benefit more from transplantation than from dialysis based on demographic information, but are never referred for a transplant evaluation [10]. So even though the waiting list for a kidney now exceeds 90,000 candidates, this may represent less than half of the true number of patients who might benefit from kidney transplantation.
Understanding the fact that efforts to increase the supply of kidneys as well as reduce (or downplay) the growing demand have been unsuccessful is crucial to understanding the key impetus for the third policy approach: revising how kidneys are allocated. Organ allocation from deceased donors is already a zero-sum affair, since any organ allocated to one candidate cannot be allocated to any other who might benefit. But a fixed supply combined with growing demand yields progressively diminishing returns because more and more candidates will be waiting longer for an organ, which in turn means that more medically suitable candidates will be sicker at the time of transplantation (resulting in worse outcomes) and more medically suitable candidates will become too sick to receive a transplant at all or will die on the waiting list.
The Proposed System
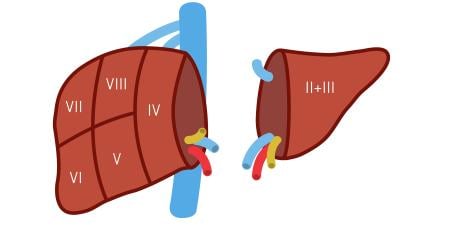
Proponents of changing kidney allocation are animated by the concern that the expanded-criteria allocation system is inefficient because it transplants kidneys of lower quality, which results in higher rates of discard, and wasteful because it allocates kidneys from young and healthy donors to older and sicker recipients. What is proposed instead is a hybrid system comprising accrued waiting time, age-matching between the donor and candidate, and a utility score based on demographic information on donors (the kidney donor profile index or KDPI) and candidates (called the estimated posttransplant survival score or EPTS).
By matching the “best” 20 percent of kidneys (as measured by KDPI) with the “best” candidates (as measured by the EPTS), and by age-matching the donor kidney to within 15 years of the age of the candidate, proponents contend [11] that the new allocation system would substantially increase total life-years accrued from all available organs. However, minutes from the August/September 2011 meeting of the UNOS/OPTN Kidney Committee report conclusions from HHS counsel that age-matching would run afoul of the Age Discrimination Act of 1975 [12]. This means that it is unlikely that explicit age-matching will be a part of any proposed revision, though donor and candidate age will probably be included as surrogate variables for predicting graft and patient survival.
Much of the conversation about the new allocation system begins by granting the premise that the scoring systems employed to match “best organ” to “best candidate” are reliable predictors of prognosis. But, as my colleagues and I have argued in detail elsewhere, there is good reason to think this is not the case [13]. If the scoring system employed in the new allocation system does not fare well as a prognostic tool, then discussing the moral defensibility of such a scoring system is premature. The practical implications of using a scoring system that may generate an incorrect prognosis of graft survival more than 30 to 40 percent of the time must be discussed first.
For starters, it is implausible that a scoring system with this degree of prognostic disability will reduce rates of organs deemed unacceptable for transplant. Transplant centers cultivate different institutional attitudes to risk. Some centers are more willing to routinely accept and transplant higher risk kidneys from physiologically marginal donors than others. These are the considered judgments of professionals, and it is implausible that the introduction of KDPI, with these stipulated prognostic limitations, would generate wholesale changes in how centers adjudicate donor risk. In any event, centers are already required to submit parameters for acceptable organ offer to UNOS/OPTN so as to avoid the inefficiency of offering a center organs that are outside its established risk tolerance [14]. The addition of KDPI to this requirement would only add confusion in instances in which it wasn’t otherwise merely redundant.
Proponents of the new allocation system are also motivated by the plight of younger patients on the waiting list, the prospect that these candidates are harmed by longer waiting times, and the potential pressures to accept a kidney of poorer quality and face the need for retransplantation. One might gather that there are legions of young people being added to the list, only to languish. But the waiting list is not evenly distributed across age cohorts.
ESRD is increasingly a disease of aging, and this is reflected both in the rising median age of newly listed candidates and in the facts that two-thirds of candidates listed for transplant are over the age of 50 and only 10 percent of listed candidates are aged 18-34. New additions to the waiting list in 2010 are distributed in roughly the same proportions [15]. So stipulating the general premise that older candidates are more likely to die on the waiting list than younger candidates and that the organ supply is zero-sum, a proposal that prioritizes younger candidates over older candidates will mean that (a) older candidates, who make up most of the waiting list, will have fewer opportunities to receive a transplant from a deceased donor (see figure 1) and (b) because older candidates are less physiologically robust, the result will be more removals from the list due to deterioration and higher rates of death on the waiting list than in the current system.
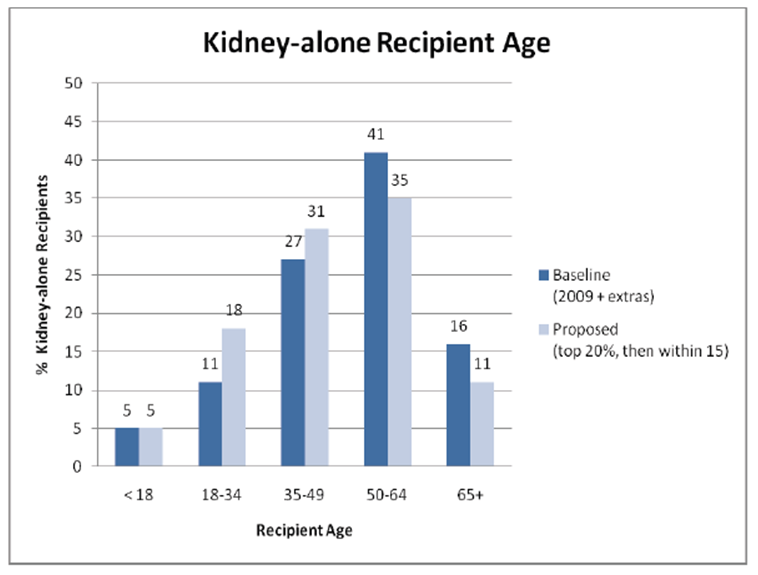
Figure 1. The ages of kidney recipients.
Proponents of the proposed system respond that this possibility will increase the pressure to use kidneys from more physiologically marginal deceased donors, pointing to the “old-for-old” program employed by the Eurotransplant Senior Program (ESP) as a favorable example. But the outcomes data from ESP suggest a less sanguine lesson. Frei and colleagues [16] reviewed 6-year patient and graft survival comparing three allocation strategies: (a) old-donor kidney to old candidate, (b) old-donor kidney to any-age candidate, and (c) any-age-donor kidney to old candidate. The results showed that old-to-old conferred significantly worse patient survival and worse graft survival than the other allocation strategies.
This should not be a surprise: kidneys from physiologically marginal donors tend to have higher rates of primary nonfunction and delayed graft function and shorter half-lives than kidneys from younger, healthier donors. In the immunosuppressed recipient, these complications confer significant risk for additional complications: infection, debilitation, and death. Old candidates are much less likely to withstand these complications than younger candidates, and so it is unsurprising that older candidates who receive marginal kidneys are more likely to sustain adverse outcomes than younger candidates.
Furthermore, preferentially allocating the “best” deceased donor kidneys to the youngest recipients may have a dampening effect on rates of living donation to young, healthy recipients, a phenomenon observed when pediatric candidates were given preferential access to organs from deceased donors less than 35 years of age [13]. Since most organs from living donors are directly donated to younger recipients in the first place, preferential allocation of deceased-donor organs may have the undesirable effect of depressing total rates of living kidney donation.
Rearranging the Deck Chairs
One hypothesis that explains why the total rate of growth of kidneys procured from deceased donors is flat to falling is that transplant centers are increasingly aware of all this. Virtually all of the growth in the deceased-donor list has come from an increase in kidney procurement from physiologically marginal donors, with a smaller fraction from donors after circulatory death. Centers are held accountable for patient and graft survival rates by UNOS/OPTN, as well as by insurers. While those survival statistics are “risk-adjusted” to account for donor characteristics and candidate comorbidities, what risk-adjustment really amounts to is, across all transplant centers, a quiet lowering of expectations for patient and graft survival.
The ongoing disagreement over the merits and flaws of different allocation regimes exposes a deeper, existential question for regulators, insurers, and the transplant community at large. The promises of efficiency and allocating “the right kidney to the right recipient” are based on empirically dubious promises of gains. The transplant community and those it treats would be far better served if the following premise was simply conceded: it actually doesn’t matter overly much whether or not the current allocation system is maintained or a new one is adopted. The fact is, so long as the growth in the organ supply is primarily from lower-quality organs from deceased donors, we can perform fewer transplants with better outcomes, or more transplants with worse outcomes, but the available data strongly suggest that we really can’t promise both more transplants and better outcomes. The transplant community should just admit that this is the crucial policy choice.
In practice, the choice between volume and outcomes will probably not be made by changes to OPTN allocation policies, but by the aggregate clinical behavior of individual transplant centers, strongly determined by their attitudes toward risk. And if, as in the past, the Health Resources and Services Administration remains unwilling to grant additional regulatory dispensation for worse reported outcomes from centers with a higher operational risk tolerance, the coming years will see fewer total kidneys procured from deceased donors, and most of that attrition will be from a reduction in the total number of kidneys transplanted from physiologically marginal deceased donors. Centers with conservative risk tolerance will remain conservative, and more centers that are currently less risk-adverse will become skeptical that this approach can be reliably offset by risk adjustments for donor and candidate comorbidities. More centers will make the calculation that by lowering their risk tolerance and doing fewer transplants with better-quality organs (which should more reliably confer better outcomes), they can escape the slings and arrows of additional scrutiny by regulators and insurers. If this comes to pass, we can expect fewer kidney transplants from deceased donors in the near future and more removals from the waiting list due to deterioration or death.
Eventually, it will become obvious that rearranging deck chairs does not yield substantially more places to sit down. The controversies over allocation really represent intellectual exhaustion in the face of a long series of inadequate policy responses to the decade-long trend of the kidney supply increasing only at the expense of organ quality and patient outcomes, exacerbated by a steady growth in demand for organs. The sooner the transplant community understands that we can’t allocate our way out of this problem, the better off our patients will be.
References
-
Organ Procurement and Transplantation Network (OPTN), Scientific Registry of Transplant Recipients (SRTR). Table 2.2 deceased donor characteristics 2000-2009. OPTN/SRTR 2010 Annual Data Report. Rockville, MD: Department of Health and Human Services; 2011. http://www.srtr.org/annual_reports/2010/default.htm. Accessed January 25, 2012.
-
OPTN/SRTR, Table 2.9 living donor characteristics, 2000 to 2009.
-
Paired kidney donation involves living donor and recipient pairs in which the donor is immunologically incompatible or is otherwise technically unsuitable to donate to their designated recipient. Incompatible pairs can be matched with other incompatible pairs, and the donor for one pair can donate to the recipient in the other pair, and vice-versa. Donor “chains” begin with a nondirected living donation—that is, when a living donor without a designated recipient volunteers to donate a kidney. When combined with paired exchange, this nondirected donation initiates and “unlocks” a series of paired exchanges. See: Rees MA, Kopke JE, Pelletier RP. A nonsimultaneous, extended, altruistic-donor chain. New Engl J Med. 360(11):1096-1101.
-
OPTN/SRTR, Figure 3.5 paired kidney donations, 16.
-
Hippen BE, Matas A. Incentives for organ donation in the United States: feasible alternative or forthcoming apocalypse? Curr Opin Organ Transplant. 2009;14(2):140-146.
-
US Renal Data System. 2011 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2011: vol. 2, 184. http://www.usrds.org/2011/view/v2_01.asp. Accessed January 25, 2012.
- Delmonico FL, McBride MA. Analysis of the wait list and deaths among candidates waiting for a kidney transplant. Transplantation. 2008;86(12):1678-1683.
-
Stone G, Pirone J. One-third of potential organ recipients ineligible. ABC News. http://abcnews.go.com/GMA/Story?id=4503954&page=1#.TyChYJgmyeg. Accessed January 25, 2012.
-
Hippen B, Satel S. Code red. National Review.http://www.nationalreview.com/articles/224180/code-red/sally-satel. Accessed January 25, 2012.
- Schold J, Srinivas TR, Kayler LK, Meier-Kriesche HU. The overlapping risk profile between dialysis patients listed and not listed for renal transplantation. Am J Transplant. 2008;8(1):58-68.
- Leichtman A, McCullough KP, Wolfe RA. Improving the allocation system for deceased-donor kidneys. New Engl J Med. 2011;364(14):1287-1289.
-
OPTN/UNOS Kidney transplantation committee. Report to the board of directors, November 14-15, 2011. http://optn.transplant.hrsa.gov/CommitteeReports/board_main_KidneyTransplantationCommittee_11_17_2011_17_29.pdf. Accessed January 25, 2012
- Hippen B, Thistlethwaite JR Jr, Ross LF. Risk, prognosis and unintended consequences in kidney allocation. New Engl J Med. 2011;364(14):1285-1287.
- Gerber DA, Arrington CJ, Taranto SE, Baker T, Sung RS. DonorNet and the potential effects on organ utilization. Am J Transplant. 2010;10(4 Pt 2):1081-1089.
-
As of January 20, 2012, there were 9,043 candidates aged 18-34 on the waiting list, compared to 24,132 aged 35-49, 39,050 aged 50-64, and 17,581 over age 65. See: Organ Procurement and Transplantation Network. Current U.S. waiting list: organ by age. http://optn.transplant.hrsa.gov/latestData/rptData.asp. Accessed January 28, 2012.
- Frei U, Noeldeke J, Machold-Fabrizii V, et al. Prospective age-matching in elderly kidney transplant recipients--a 50-year analysis of the Eurotransplant Senior Program. Am J Transplant. 2008;8(1):50-57.